Data shows Cigna’s oncology case management program’s distress screening tool improves engagement and lowers costs.

Data shows Cigna’s oncology case management program’s distress screening tool improves engagement and lowers costs.
A cancer diagnosis is life-altering and feelings of distress, or an inability to cope, are common reactions. In fact, almost half of all people with cancer experience clinically significant distress throughout their disease and treatment journey.
Helping people with cancer identify their level of emotional distress, and connecting them to resources that support their whole-person health, can have a powerful effect on their health, well-being and costs of care.
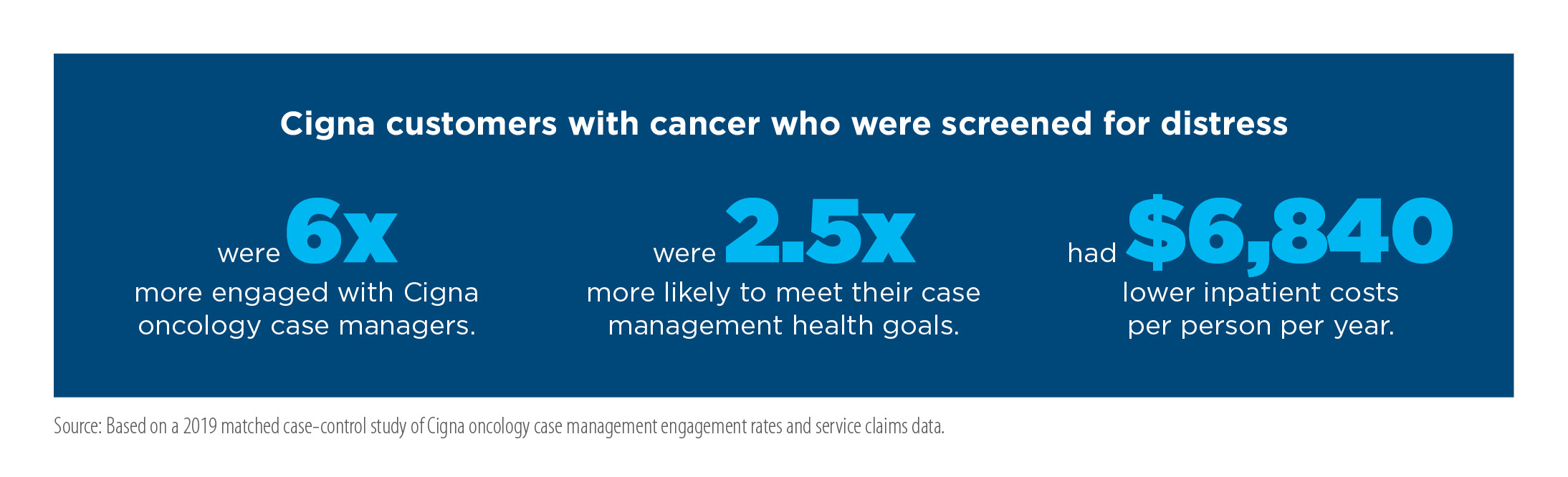
People who received distress screening and resource referrals from Cigna’s leading oncology case management program have shown six times higher program engagement rates and an average savings of $6,840 in annual care costs per person. That’s according to a 2019 Cigna analysis of case management engagement rates and inpatient service claims data from September 1, 2016 through June 1, 2018 for 2,176 Cigna health care commercial customers who had been diagnosed with a cancer condition and participated in Cigna’s oncology case management program. “Living with cancer can feel overwhelming and emotional distress is expected, but it can lead to problems if left unmanaged,” said Bhuvana Sagar, MD, medical oncologist and national medical executive for Cigna. “Distress can negatively affect how a person copes with their condition and functions during their everyday life, including the decisions they make that can affect their treatment and overall health.”
“Distress screening for people with cancer is vital, and has been found to help improve acceptance of their condition and adherence to treatment,” said Alysia Swanson, clinical program senior advisor for Cigna. Psychosocial distress screening was added to the American College of Surgeons Commission on Cancer accreditation standards in 2012, but for years many patients went unscreened due to the difficulty of incorporating screening protocols into provider workflows.
To help fulfill the need for effective screening, Cigna formed an integrated team of behavioral, medical, and pharmacy experts to implement a distress screening tool for customers in cancer treatment through oncology case management services. These services are provided by a dedicated team of Cigna oncology nurses who offer personal assistance and support people during the treatment journey. Cigna oncology case managers are trained nurses who have a current nursing license in at least one state. When working as a case manager, they are not practicing nursing or giving medical advice.
Specialized Case Management Delivers Personalized Cancer Support
Cigna’s oncology case management program helps people diagnosed with cancer ease their treatment journey, reduce complications, and lower care costs through personalized support and coordination of care.
A dedicated oncology case manager, who is a specially trained oncology nurse, supports people at every step of cancer treatment. Case managers work with patients, their family, the treating oncologist, and the extended care team to help people better understand their condition, navigate treatment options, and maximize use of their health plan benefits so they can connect to high quality care in the most affordable and convenient way possible. Case managers also provide referrals to a network of support staff including social workers, pharmacists and behavioral clinicians, as well as to helpful services and local resources designed to address social needs and help people ease the emotional turmoil that often occurs during cancer treatment.
These specialty case managers are part of an integrated support team that includes medical directors with extensive oncology experience. Their approach to oncology case management aims to address each individual’s whole-person health needs by delivering holistic support, value-based quality care, and personalized, affordable therapy — leading to greater individual well-being and medical cost savings.
Distress screening and support is just one of the many cost savings drivers from Cigna oncology case management. Overall, medical costs are $13,704 lower per person for those engaged in the program for two years, according to Cigna Global Data Analytics program evaluation, September 2020 (medical cost savings accrue in the year after treatment).
Below we look at the results of Cigna’s data analysis and explore how effective identification and support for distress can lead to a better quality of life and lower cost of care.
More Involvement in Case Management Leads to Inpatient Cost Savings
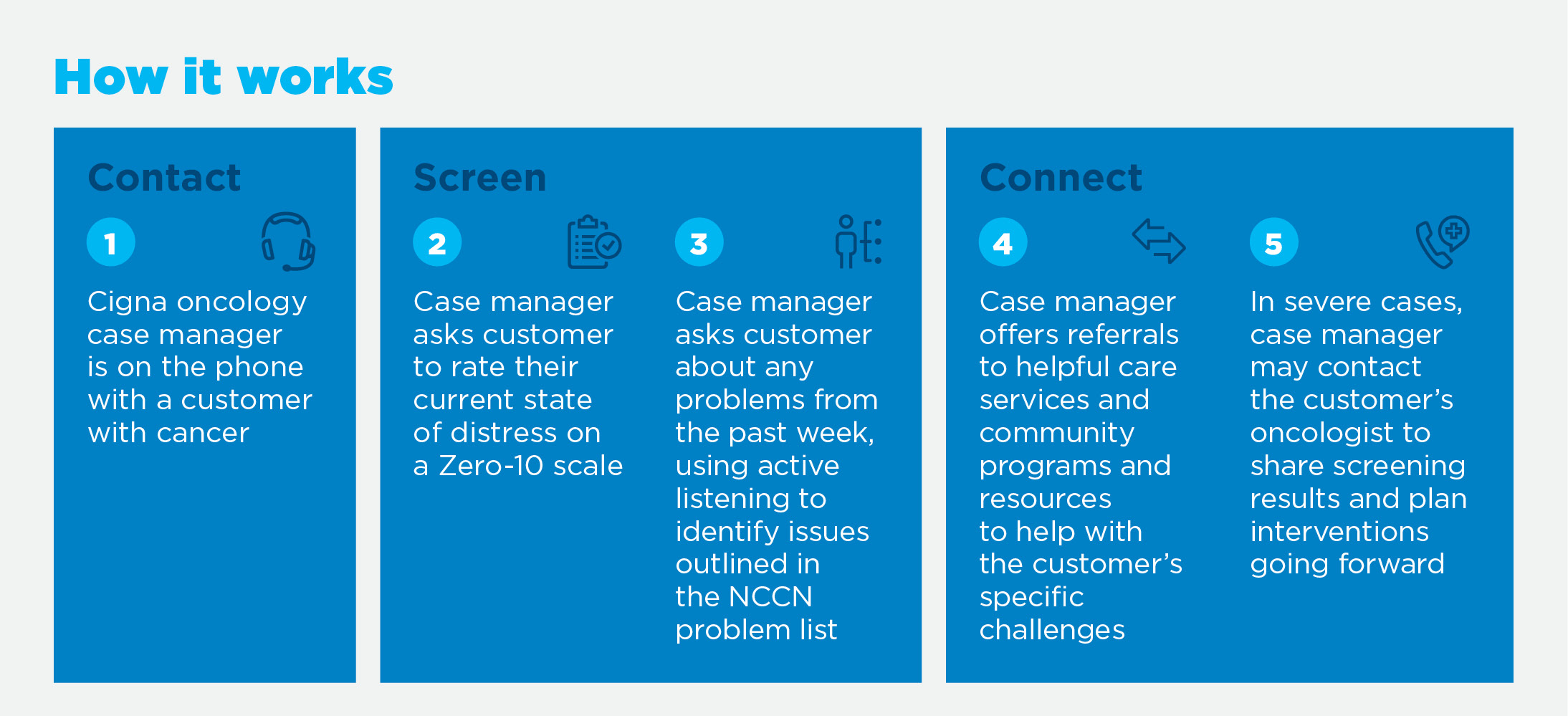
Distress screening is used by Cigna oncology case managers when they first connect with a customer with cancer and again during pivotal changes in the treatment journey. Additional screenings may be conducted based on the individual’s particular needs and the case manager’s discretion.
According to Cigna's 2019 data analysis, the use of distress screening and interventions yields significant results. In one year alone, customer engagement rates were six times higher among those who were screened than those who were not screened. The screened customers also engaged with case managers for a 167% longer time period, or an extra 73 days, on average (184 days vs. 110 days for unscreened customers).
“We have seen that longer and more sustained engagement between a case manager and a customer has a higher likelihood of success,” said Swanson. “Our distress screening tool supports a more comprehensive conversation about their medical, behavioral, and physical health experience, which in turn supports adherence with care plan goals. This can lead to better clinical and cost results over time.”
Indeed, Cigna's 2019 data shows that customers screened for distress were 16% more likely to be referred to services and resources to address areas of concern. These referrals include behavioral health services to help customers manage distress. The analysis showed that screened customers were 1.3 times more likely to use behavioral health services and 2.5 times more likely to meet their health goals set with their case manager (38.2% of screened customers met their goals vs. 15.4% of unscreened customers).
What’s more, the 2019 claims analysis of customers engaged in oncology case management revealed that distress screening can reduce inpatient costs by $6,840 per person in one year. This reduction was largely driven by a 10.4% decrease in the number of customers needing an additional inpatient visit, and an average of 14.7% fewer inpatient visits overall.

Screening for Distress Using a Clinically Validated Tool
The Cigna distress screening tool was adapted from the screener created by the National Comprehensive Cancer Network (NCCN), a nonprofit alliance of the country’s leading cancer centers. The NCCN tool comprised of a 10-point scale distress thermometer and comprehensive problem list aimed at identifying physical, family, emotional, practical, and spiritual or religious concerns leading to distress. After validating NCCN’s screener per evidence-based clinical medicine, Cigna purchased the rights to use it in their oncology case management practices.
The NCCN screener was originally a pen-and-paper tool given to the patient by an oncologist or treatment provider. Cigna adapted it into a telephone format to enable case managers to quickly gauge the individual’s distress levels at every stage of treatment.
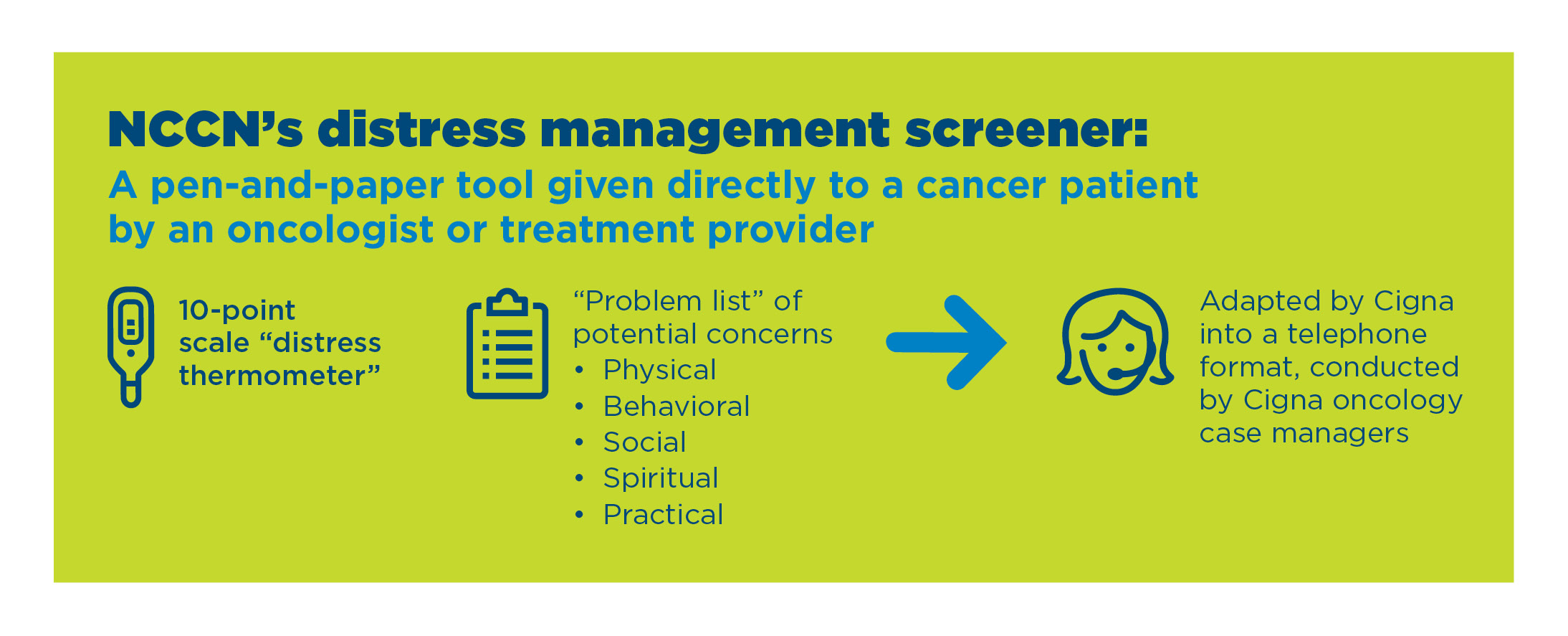
Cigna oncology case managers screen customers by asking them to measure their distress level on a scale of zero (no distress) to 10 (severe distress). They then ask the customer to share any problems or concerns experienced from the previous week up to the day of the call, using active listening to identify key issues that can be addressed with additional support services.
“With the use of this simple tool, our case management clinicians are able to assess people for distress and identify issues that are likely driving it,” Swanson said. “This enables case managers to help customers find and access available programs, services, and resources that can help them overcome these issues and enable them to better cope with the diagnosis, treatment, and overall cancer journey.”
Addressing Barriers to Care
In helping customers with cancer manage distress, oncology case managers can refer customers to helpful clinical services, including behavioral health benefits and employee assistance programs (whether offered by Cigna or elsewhere). However, more often than not, customer health issues are compounded by financial and social challenges in their lives.
“We’ve found that people often need help getting food on the table or paying utilities or medical bills,” said Sagar. “These and other factors, known as social determinants of health, can have a greater impact on health outcomes than the treatment itself.” Cigna oncology case managers use approved directories and reference tools to identify nearby resources to help customers with food and financial assistance, plus other useful services such as transportation and other community support programs.
A Broad Spectrum of Resources
Customers are connected to available services to help them cope with distress.
- Cancer and stress management education and support
- Behavioral health services
- Employee assistance programs
- Community resources, including transportation services, and food and financial assistance
- Disability support
- Social workers
- Registered dieticians
- Caregiver job aids
- Pharmacy support via medication coaching and medication reconciliation
Collaborating With Treatment Providers
The Cigna oncology case manager can notify the oncologist about the screening results, as well as the resource referrals that were offered and accepted. “In many cases this can lead to treatment plan changes that better address specific needs,” said Swanson. “The oncologist will work with the patient in the clinical setting, while the oncology case manager assists the patient by telephone to address their needs at home.”
There is opportunity to improve screener utilization and help more people. “There are reports that NCCN’s distress screening thermometer is under-utilized in many cancer provider settings,” Sagar said. “When our case managers report customer distress levels to our oncologists, we demonstrate the value of distress screening, which we hope will lead to broader implementation within the clinical practice.”
Award-Winning Results that Benefit Plan Sponsors and the People We Both Serve
Actively detecting and addressing distress helps create a more positive experience during the cancer journey. As a result, people are more likely to adhere to their course of treatment and less likely to use avoidable medical services — demonstrating improved management of individual health and lower costs. Cigna’s successful adaptation of the NCCN distress screening tool was recognized by the National Alliance of Healthcare Purchasers Coalition’s 2021 eValue8 Innovation Award.
Based on the results, Cigna has expanded utilization of distress screening and now includes it as part of case management for customers facing other complex health issues, including those undergoing a transplant, taking specialty medications, and accessing gene and cell therapies. “We are continuously evaluating utilization as well as the clinical and cost benefits to customers, and are exploring other ways to further expand the use of distress screening across other case management services,” said Swanson.